Optimising Toothbrushing in Nurseries and Schools
A quarter of five-year-old children in England have tooth decay – rising to up to 50% in areas of deprivation. The burden of decay is significant, causing pain and suffering, affecting what children eat, their speech, quality of life, self-esteem, and social confidence.
In addition, decay has a wider societal impact on school readiness and attendance. In England, treatment of decay is the most common reason why more than 33,000 young children every year are admitted to hospital, costing the NHS over £40 million annually.
A key behaviour in preventing decay is toothbrushing with a fluoride toothpaste. Supervised toothbrushing programmes in nurseries and schools do not replace toothbrushing at home but serves to complement home toothbrushing to help young children learn and practice good oral hygiene.
Nursery and school-based supervised toothbrushing programmes can be effective, especially in children at greatest risk, and are cost effective. However, uptake and maintenance of these programmes is fragmented, with funding coming from a variety of sources, and there is considerable variation in how they are implemented.
To combat this, the BRUSH Project, co-led by Professor Peter Day and Dr Kara Gray-Burrows at the University of Leeds, and Professor Zoe Marshman at the University of Sheffield, provides an evidence-based toolkit to support the implementation of supervised toothbrushing programmes and clubs in England.
The toolkit includes all the resources necessary to establish a supervised toothbrushing programme, including how to navigate the commissioning and procurement process; how to set up, run and evaluate the programme; training and promotion, as well as focused information for early years settings and parents.
 It was co-designed by academics and stakeholders at all levels of implementation following an extensive research programme which started with a review of existing supervised toothbrushing programmes in 2022, taking information from 141 local authorities across England.
It was co-designed by academics and stakeholders at all levels of implementation following an extensive research programme which started with a review of existing supervised toothbrushing programmes in 2022, taking information from 141 local authorities across England.
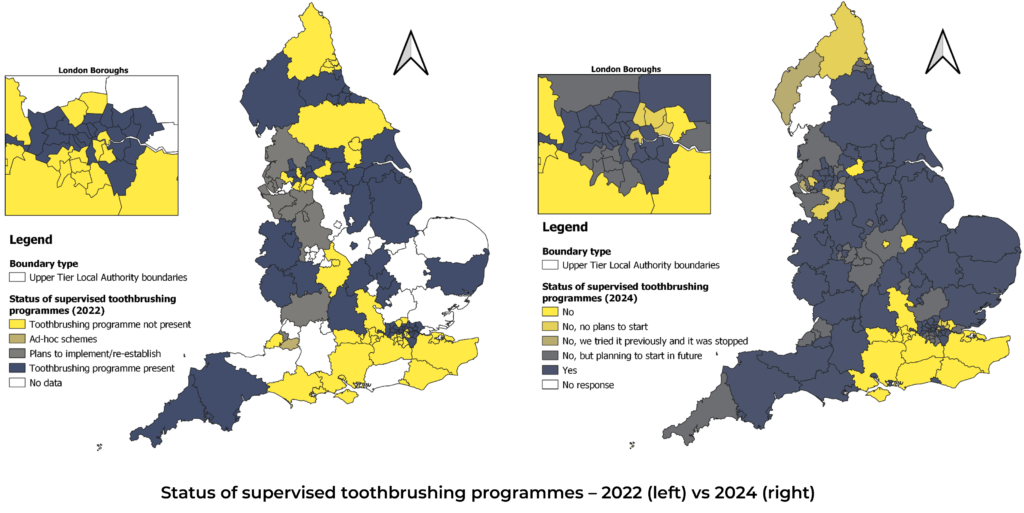
This data was used to produce geographical mapping of programmes across England, including variables such as deprivation level; levels of tooth decay in children; number of hospital admissions for tooth extraction under general anaesthetic; dental access; rurality, and early-years education data. This data will be reviewed over time to see how it changes, with a second survey now completed (due for publication in Winter 2024) and the third taking place in 2025.
The barriers and facilitators to implementing toothbrushing programmes were explored in-depth by researchers in interviews with 159 key stakeholders across England, including commissioners; oral health providers; nursery and school staff; parents; and children.
Researchers used this data to co-design the toolkit with stakeholders, who also took part in group sessions to discuss the findings and reflect on what resources are already available, their quality, and identify gaps to aid implementation.
The toolkit was piloted before being made available to download for free; it has received over 10,000 unique visitors since January 2024. The research team is working with a number of national and local bodies to discuss its findings and inform local and national policy, including the Department of Health and Social Care, the Department for Education, NHS England Transformation Programme Team for Oral Health, and Local Government Association.
Facts & Figures
- A quarter of five-year-old children in England have tooth decay – rising to up to 50% in areas of deprivation.
- In England, treatment of decay is the most common reason why more than 33,000 young children every year are admitted to hospital, costing the NHS over £40 million annually.
- Nursery and school-based supervised toothbrushing programmes can be effective, especially in children at greatest risk, and are cost effective. However, uptake and maintenance of these programmes is fragmented with funding coming from a variety of sources, and there is considerable variation in how they are implemented.
Links